Curriculum Content and Overview
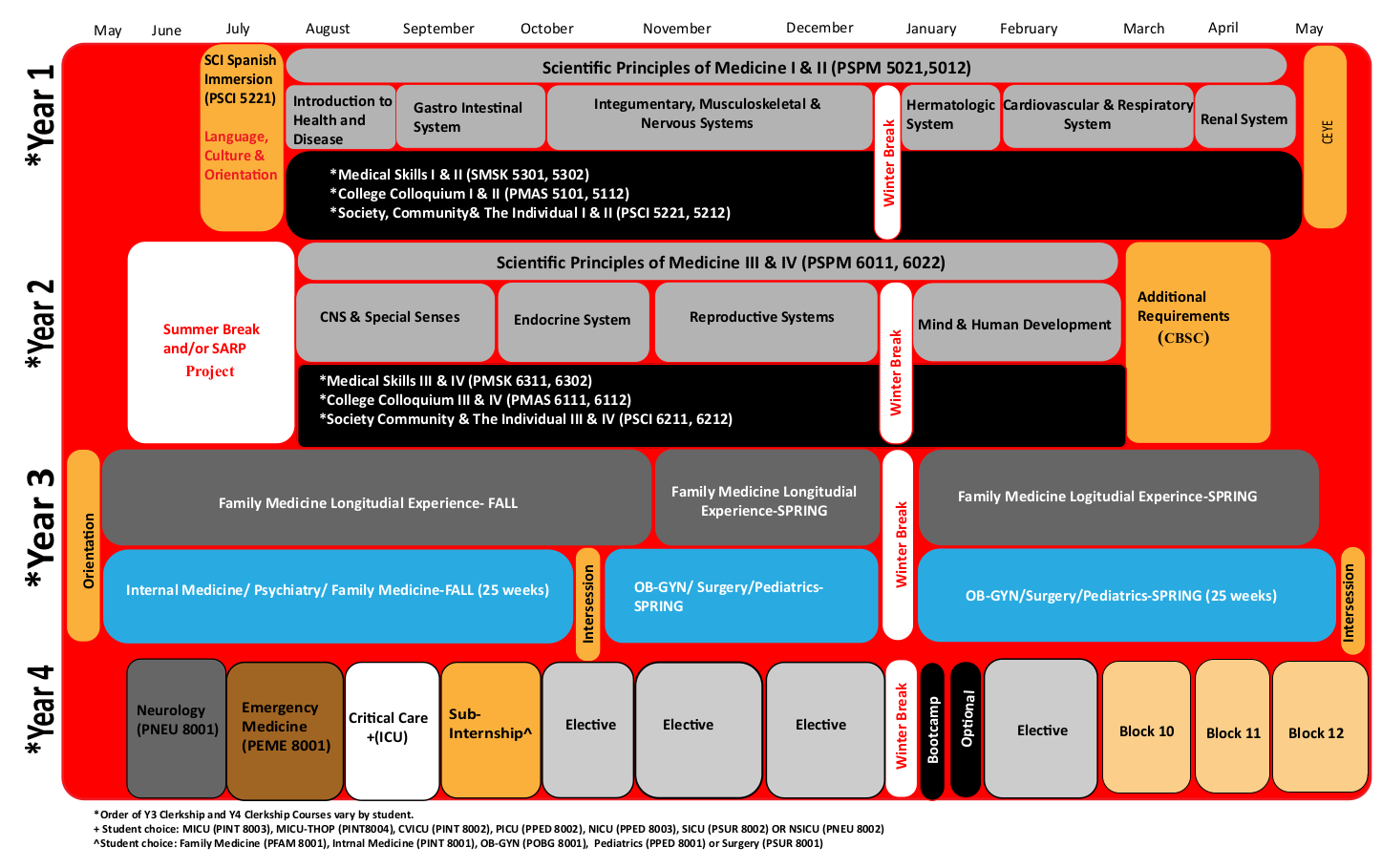
The Paul L. Foster School of Medicine has established a highly integrated, clinically orientated approach to teaching and learning for its four year M.D. degree program. Through the integration of the basic and clinical sciences from the onset of instruction, students learn anatomy, biochemistry, physiology, and other basic science concepts and are presented with the content needed to understand specific clinical presentations. This method provides learners with increased understanding, content retention, meaningful connections of basic science to clinical practice, and accelerates the attainment of diagnostic reasoning skills.
The pre-clerkship curriculum consists of four required courses: Scientific Principles of Medicine (SPM); Medical Skills; Society, Community, and the Individual; and Masters’ Colloquium. In addition, students participate in one longitudinal experience via the Scholarly Activity and Research Program (SARP).
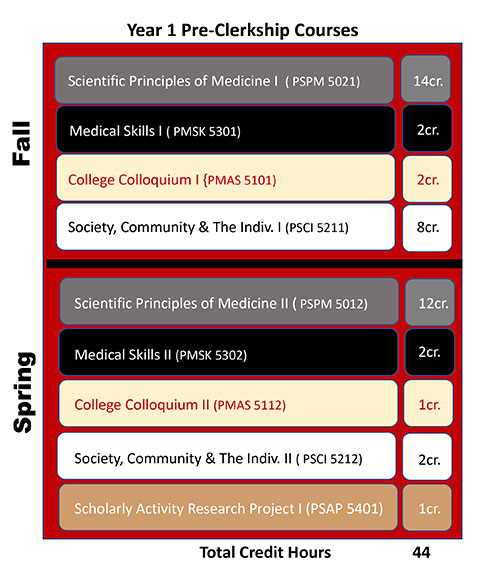
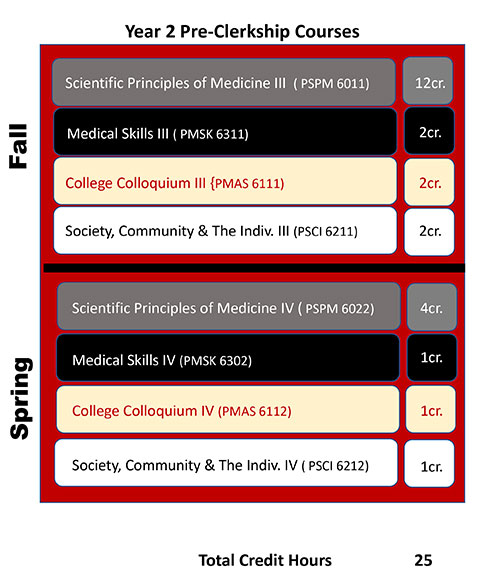
Four of these courses span the first two years of the curriculum and are highly integrated with one another. The centerpiece of the curriculum is Scientific Principles of Medicine (PSPM 5021, 2012, 6011, 6022), which is organized around roughly 77 clinical presentations (e.g., sore throat, abdominal pain, chest discomfort) that are assigned to an appropriate organ system block or unit. Each of the clinical presentations (CPs) is delivered to students by an expert clinician faculty member in the form of a clinical scheme that serves as the basis for the instruction in the basic science concepts and content relevant to an understanding of the pathophysiological processes associated with a given clinical presentation.
Closely aligned with SPM, is the Medical Skills (PMSK 5301, 5302, 6311, 6302) course where students learn to take focused histories and conduct physical examinations on patients presenting with the clinical problems that are being addressed concurrently in SPM. For example, when learning the basic sciences relevant to understanding chest discomfort in SPM, Medical Skills covers how to take histories and perform physical examinations on standardized patients presenting with chest pain. This course takes place primarily in a state-of-the-art clinical skills and simulation laboratory where students practice with standardized patients, partial task-trainers, and high-fidelity human body simulators.
The Society, Community, and the Individual: The Integration of Public Health and Community Medicine (PSCI 5221, 5212, 6211, 6212) course is taught by an interdisciplinary team of faculty representing medicine and public health. SCI focuses on population health (e.g., epidemiology, bioinformatics, and evidence-based medicine) knowledge and skills needed to apply the scientific method to research design and the selection and application of appropriate statistical tests. Community health and health promotion methods are examined along with issues related to public health policy and advocacy. This course integrates medicine and public healthy providing an arena that enhances Spanish language skills, provides an opportunity to experience community medicine and community visits while interacting with members of a healthcare team, and gives students the chance to experience culturally diverse populations. These community experiences help students to develop behaviors and attitudes required to work collaboratively with other health care professionals and community members. The course also provides opportunities for students to apply the tools of information technology in conducting literature searches, interpreting and critiquing scientific articles, weighing evidence, and practicing evidence-based medicine. As appropriate, SCI is integrated with the systems-based SPM/Medical Skills units and topical issues explored with the College Colloquium.
The fourth major course spanning the first two years of the curriculum is College Colloquium (PMAS 5101, 5112, 6111, 6112). The PLFSOM has created learning communities called “Colleges,” led by college colloquium. The college colloquium are responsible for organizing a weekly college colloquium focusing on the art and science of medicine with specific emphasis on issues related to professionalism. The colloquium is primarily a discussion-based course with selected readings and in-class exercises designed to promote critical reflection and the exchange of ideas.
The organization of the third and fourth year clerkship curriculum is illustrated in the following schematics:
Clerkship Phase
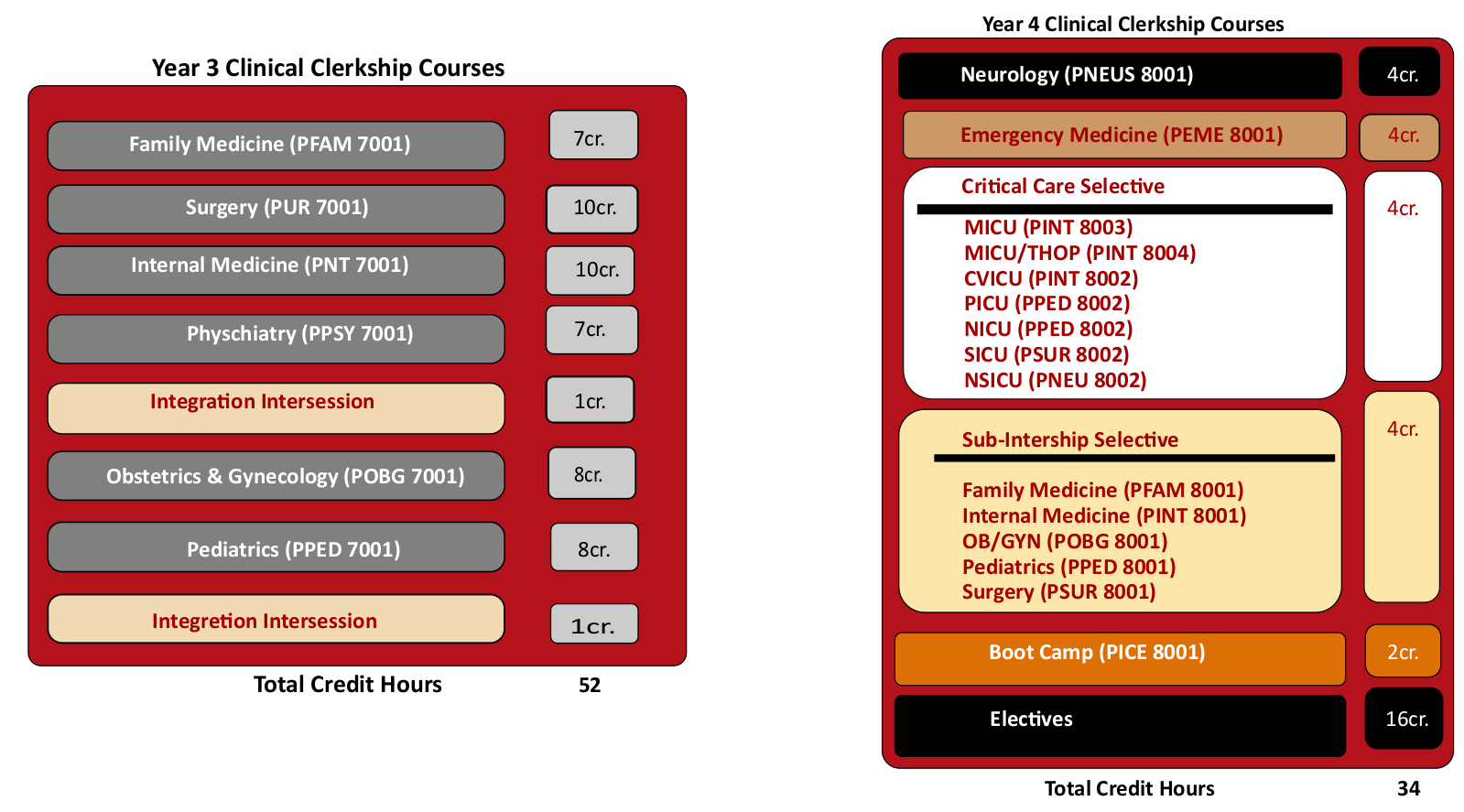
Year 3 Curriculum
The third-year curriculum is based on a blended longitudinal integrated clerkship model. The year consists of two 23-week clerkship blocks and 4 weeks of Intersession interspersed with one week at the beginning of each block and 2 weeks at the end of the academic year. Block 1 includes concentrations in Internal Medicine, Psychiatry, Family Medicine and. Block 2 includes concentrations in Obstetrics and Gynecology, Pediatrics and Surgery. The blocks are designed to include cross-disciplinary, integrated and shared teaching instructional experiences. Half of the students begin in Block1 and half in Block 2 and then rotate at the end of the fall semester. In addition, longitudinal clinical experiences in Family Medicine and Emergency Medicine span across the entire year. Note that while several disciplines are covered simultaneously within each block, students receive individual grades for each clerkship.
The schedule each semester contains concentrated time for inpatient rotations and time for ambulatory clinic rotations. Subspecialty selectives are built into the schedule. Parallel streaming of experiences during ambulatory rotations builds on the concept of interleaving in adult learning theory. Open space is flexible time built into the calendar and can be used for study, follow-up of continuity patients or personal time. The Intersessions are used for shared activities, trainings and end-of-year testing. The entire class participates in the activities. Intersession content also ties together the experiences in the clinical rotations during year three with concepts from the first- and second-year basic science coursework.
Integrated Clerkships provide added educational value by including opportunities to not only learn more about each specialty, but also obtain medical knowledge and skills on a broader and deeper level. The information learned in each specialty builds and enhances future learning as students move through the Blocks. For example, the MSIII Obstetrics and Gynecology, Pediatrics and Surgery Block covers a full semester in which the student will have an opportunity to integrate teaching and learning experiences across the three disciplines, observing the developmental continuum from prenatal to postnatal life and gaining an understanding of medical and surgical treatment options for patients of all ages with a variety of conditions. During the perinatal period, medical decisions made by the mother will impact the infant, and the medical condition of the infant can affect the health of the mother. Psychosocial aspects of family life prior to and during the pregnancy are important in the care of the child. A holistic approach is important in all disciplines. When considering treatment options, gynecologic surgeons and general surgeons take a comprehensive approach that goes beyond the operating room with attention to quality care in the pre-operative and post-operative periods. Students will also appreciate the inter-professionalism and interdisciplinary approaches they work with and observe other disciplines, such as social work and pharmacy, to enhance patient care and safety.
The overall goal of each block is to encourage students to think about patient problems from the standpoint of multiple disciplines and perspectives. In addition, each of the blocks is designed to revisit a number of the clinical presentations (CPs) from pre-clerkship phase, reinforcing basic scientific concepts and diagnostic reasoning, with additional emphasis placed on treatment and management considerations. As part of the end-of-block assessment, students participate in a multi-station Objective Structured Clinical Examination (OSCE) that presents integrated cases (e.g., an anxious patient presenting with chest pain, a pregnant adolescent, preoperative assessment of an elderly patient, etc.). Finally, the following topics are threaded throughout the required components of years three and four: geriatrics, basic science correlations, ethics, professionalism, evidence-based medicine, patient safety, pain management, palliative care, quality improvement, communication skills, diagnostic imaging, clinical pathology and clinical research.
Year 4 Curriculum
The fourth-year curriculum is flexible and student-centered with a focus on preparation for the first day of residency. The fourth year consists of required courses, electives (both home and away) and flexible time. Required experiences include Emergency Medicine Clerkship, Neurology Clerkship, a Sub-Internship, Critical Care, Bootcamp and 16 weeks of electives, with a requirement for one elective in the basic sciences or research. Flexible time can be used for study, additional elective experiences, test preparation, vacation and travel for interviews for residency positions. Finally, all fourth-year students participate in a two-week-long boot camp experience designed to tie together the clerkship phase of the curriculum and to prepare them for the transition from medical student to first-year resident.
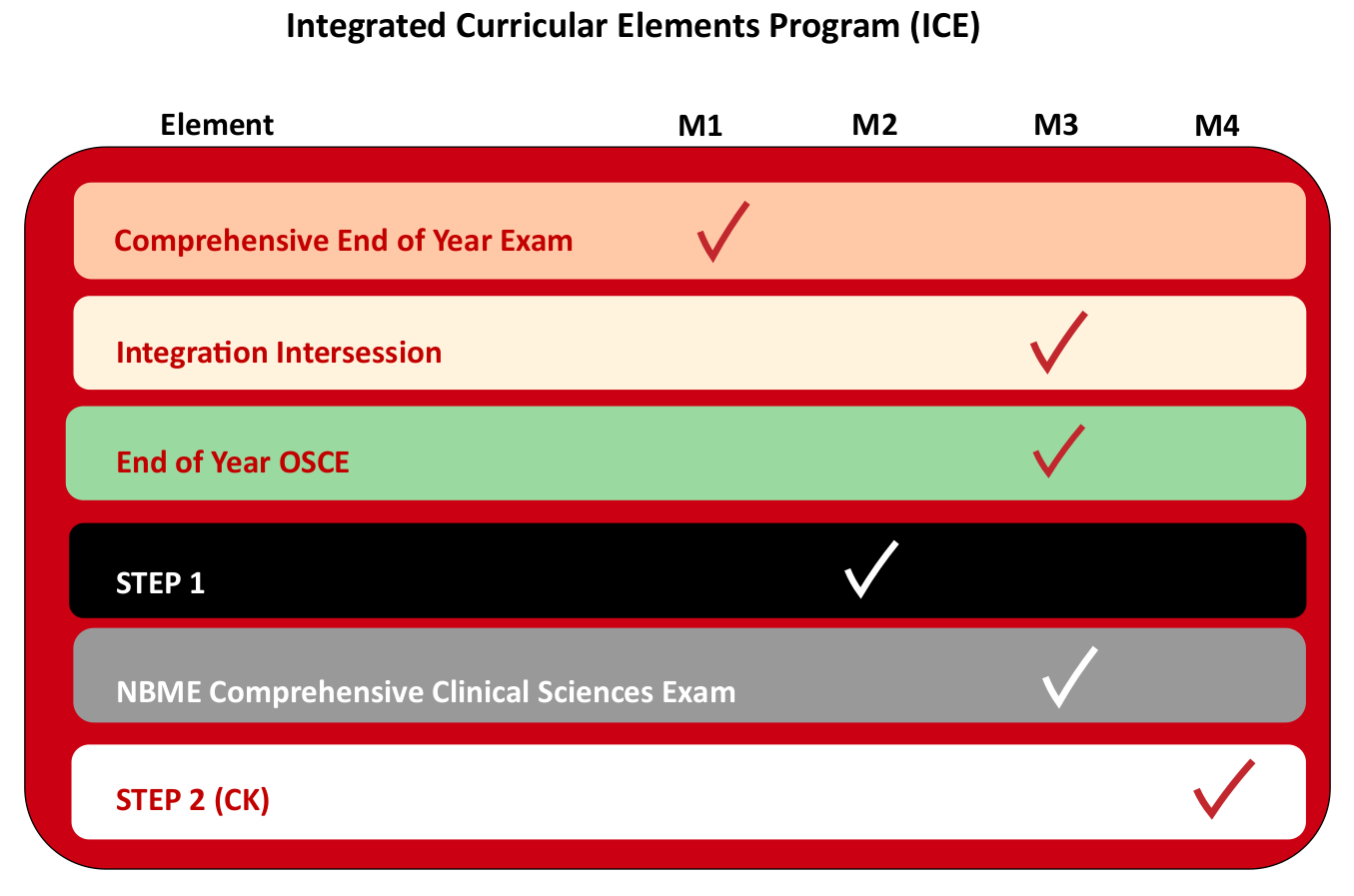
Integrated Curricular Elements Program
The integrated curricular elements are graduation requirements and students are expected to complete them as scheduled within the years as indicated and in the framework as described. As with all of the courses and requirements, please consult the relevant syllabi and descriptions in the curriculum management system for additional information.
Elements are outlined in the table below:
In addition, non-curricular elements (like holidays) may be placed on the ICE calendars so that you can plan for them.
Year 3 Intersessions:
A two week intersession course in the third year following the spring semester. The entire class will participate in the activities. Content will integrate the experiences in the clinical rotations during Year 3 with concepts from the Year1 &2 coursework.
Topics may include:
- Ethics and professionalism
- Personal reflection
- Biostatistics and Epidemiology
- Cultural competency
- Basic science material
- Integrated case presentations
- Medical skills
Content in the intercession is designed to allow for flexibility in order to adapt to the needs of the class, prepare the students for 4th year, as well as national examinations, such as the USMLE Step 2 CK.
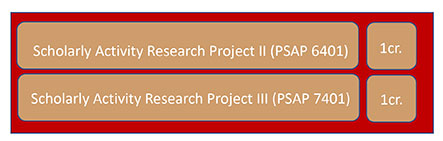
Scholarly Activity and Research Program
The Scholarly Activity and Research Program (SARP) (PSAP 5401, 6401, 7401) provides medical students with an opportunity to design and execute an independent scholarly project or research project under the guidance of a faculty mentor. A wide variety of topics and research areas are available in three broad categories, allowing for a project to be tailored to a student’s background and interests: 1) basic, clinical and translational research; 2) epidemiology, community-based, behavior, public and environmental health; and 3) medical humanities, qualitative research and medical education research. This is a three credit (pass/fail) mandatory curriculum requirement, with one credit awarded for selection of a mentor and preparation of a project plan, one credit for execution and final report of the project itself, and a final credit awarded for a poster summarizing the project presented at an annual student symposium held in the fall semester.
Students can choose between one of three tracks for completing their SARP requirement. Track 1 concentrates execution of the project into the summer between the first and second year with a final report and poster presented in the fall of the second year; whereas Track 2 provides the student more flexibility in the execution of their project with completion and final report and poster presentation in the fall of the third year. Track 3 is dedicated to completion of the SARP requirement during year four with the final report completed in fall and poster the presented in spring of year four. Students on Track 2 or Track 3 are required to submit annual progress reports until their SARP requirement is completed.
For all tracks, selection of a mentor and preparation of a project plan is due at the end of the first year. This introduction to the methodology and analytic thinking involved with scholarly activity and research is designed to enhance the medical training experience and provide an appreciation for the tight integration between scholarship, research and clinical practice. Students who excel in scholarly activities and research, based on the judgment of a faculty panel, are eligible for special recognition at graduation with the notation of graduating with Distinction in Research and Scholarship on their diploma.
The M.D. degree will be awarded to students who satisfactorily complete the following:
- all required courses and clerkships
- all graduation requirements
- passing the United States Medical Licensing Examination (USMLE) Steps 1 and 2 (Clinical Knowledge & Clinical Skills components) exams
Interprofessional Education First year medical students are required to complete the TTUHSC online course for preparation for interprofessional education. This requirement is coordinated through the Society, Community and Individual Couse (PSCI 5211) during immersion.
United States Medical Licensing Exam Policy Students are required to take Step 1 of the USMLE prior to beginning their third year and must achieve a passing score to continue to the third year. A passing score on Step 2, Clinical Knowledge, is required for graduation.