Curriculum Content and Overview
You are currently viewing the 2016–17 PLFSOM school catalog.
The Paul L. Foster School of Medicine has established a highly integrated, clinically orientated approach to teaching and learning for its four year M.D. degree program. Through the integration of the basic and clinical sciences from the onset of instruction, students learn anatomy, biochemistry, physiology, and other basic science concepts and are presented with the content needed to understand specific clinical presentations. This method provides learners with increased understanding, content retention, meaningful connections of basic science to clinical practice, and accelerates the attainment of diagnostic reasoning skills.
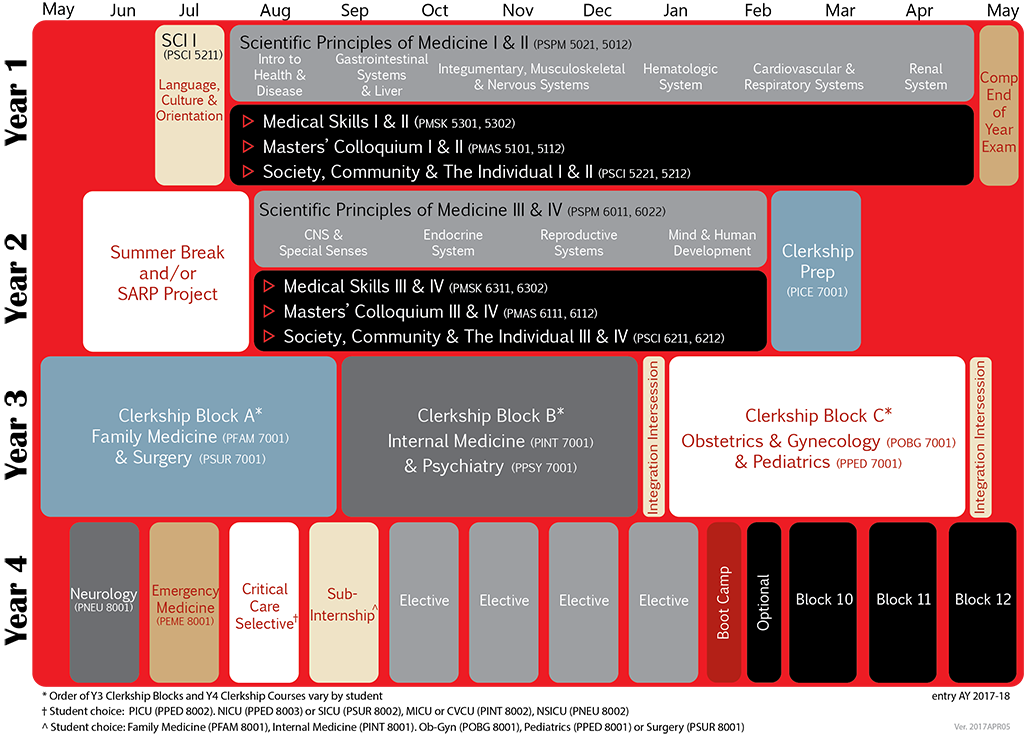
The pre-clerkship curriculum consists of four required courses: Scientific Principles of Medicine (SPM); Medical Skills; Society, Community, and the Individual; and Masters’ Colloquium. In addition, students participate in two longitudinal experiences via the Integrated Curricular Elements (ICE) Pre-Clerkship Prep Program and the Scholarly Activity and Research Program (SARP).


Four of these courses span the first two years of the curriculum and are highly integrated with one another. The centerpiece of the curriculum is Scientific Principles of Medicine (PSPM 5011, 5002, 6001, 6012), which is organized around roughly 77 clinical presentations (e.g., sore throat, abdominal pain, chest discomfort) that are assigned to an appropriate organ system block or unit. Each of the clinical presentations (CPs) is delivered to students by an expert clinician faculty member in the form of a clinical scheme that serves as the basis for the instruction in the basic science concepts and content relevant to an understanding of the pathophysiological processes associated with a given clinical presentation.
Closely aligned with SPM, is the Medical Skills (PMSK 5301, 5312, 6301, 6312) course where students learn to take focused histories and conduct physical examinations on patients presenting with the clinical problems that are being addressed concurrently in SPM. For example, when learning the basic sciences relevant to understanding chest discomfort in SPM, Medical Skills covers how to take histories and perform physical examinations on standardized patients presenting with chest pain. This course takes place primarily in a state-of-the-art clinical skills and simulation laboratory where students practice with standardized patients, partial task-trainers, and high-fidelity human body simulators.
The Society, Community, and the Individual: The Integration of Public Health and Community Medicine (PSCI 5211, 5212, 6211, 6212) course is taught by an interdisciplinary team of faculty representing medicine and public health. SCI focuses on population health (e.g., epidemiology, bioinformatics, and evidence-based medicine) knowledge and skills needed to apply the scientific method to research design and the selection and application of appropriate statistical tests. Community health and health promotion methods are examined along with issues related to public health policy and advocacy. This course integrates medicine and public health by providing an arena that enhances Spanish language skills, provides an opportunity to experience community medicine and community visits while interacting with members of a healthcare team, and gives students the chance to experience culturally diverse populations. These community experiences help students to develop behaviors and attitudes required to work collaboratively with other health care professionals and community members. The course also provides opportunities for students to apply the tools of information technology in conducting literature searches, interpreting and critiquing scientific articles, weighing evidence, and practicing evidence-based medicine. As appropriate, SCI is integrated with the systems-based SPM/Medical Skills units and topical issues explored with the Masters Colloquium.
The fourth major course spanning the first two years of the curriculum is Masters’ Colloquium (PMAS 5101, 5112, 6111, 6112). The PLFSOM has created learning communities called “Colleges,” led by College Masters. The College Masters are responsible for organizing a weekly masters’ colloquium focusing on the art and science of medicine with specific emphasis on issues related to professionalism. The colloquium is primarily a discussion-based course with selected readings and in-class exercises designed to promote critical reflection and the exchange of ideas.
The organization of the third and fourth year clerkship curriculum is illustrated in the following schematics:
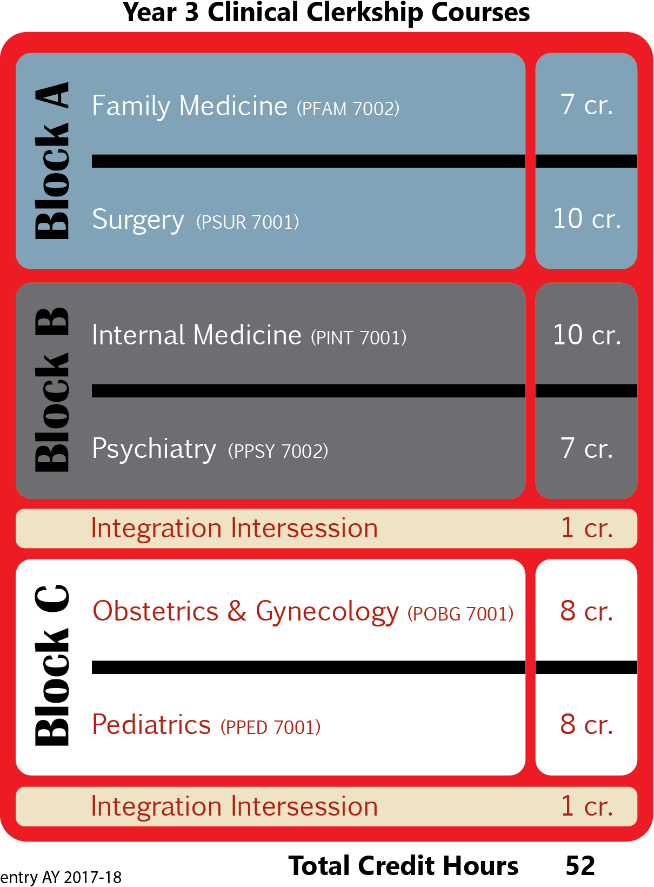
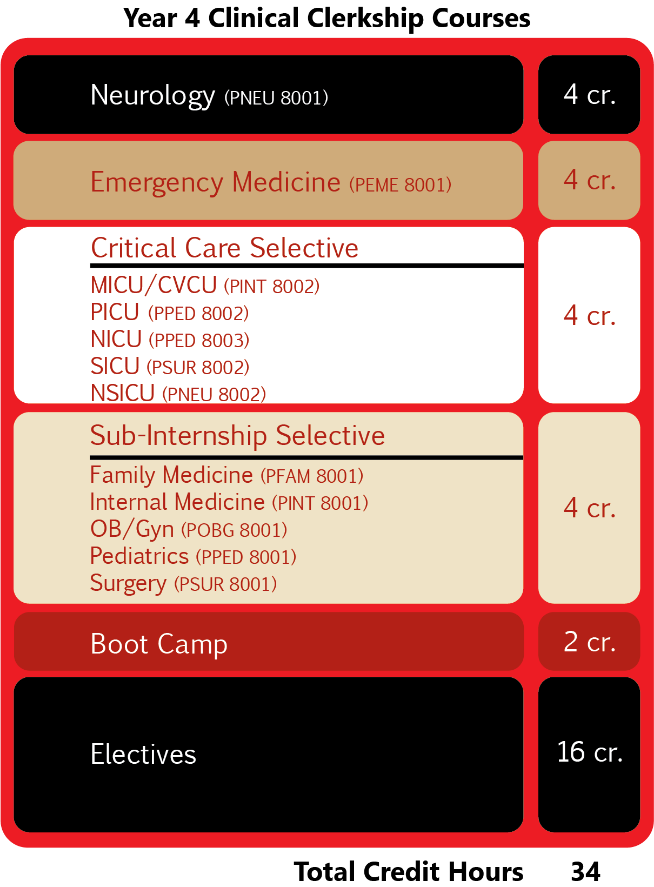
Order of Year 3 & Year 4 clerkships and coursework vary by student – requirement listing only, sequence not implied
Year 3 Curriculum
In year 3, students participate in the following clerkships: Internal Medicine (10 weeks), Family Medicine
(6 weeks), Obstetrics and Gynecology (8 weeks), Pediatrics (8 weeks), Surgery (10 weeks), and Psychiatry (6 weeks). Subspecialty “selective experiences” are built into the third year schedule in two ways: as 2-4 week blocks including both ambulatory and inpatient experiences; and in two longitudinal experiences during the Family Medicine/Surgery and Internal Medicine/Psychiatry Blocks which generally meet one half day per week in ambulatory settings. During the 16 week period in which students complete the Obstetrics and Gynecology and Pediatrics block, a Maternal/Fetal/Neonatal experience substitutes for the longitudinal selective.
Year 4 Curriculum
The fourth year curriculum, consists of four required clerkship experiences—a sub-internship, critical care medicine, emergency medicine, and neurology. During the fourth year students also are provided time for elective experiences (both at home and away) and time to travel to other medical centers to interview for residency positions. Finally, all fourth year students will participate in a two week long “boot camp” experience designed to tie together the clerkship phase of the curriculum and to prepare for the transition from medical student to first year resident.
Boot Camp
Each student will be required to participate in one two-week boot camp in the spring of their fourth year. The primary objective of the rotation will be to ensure readiness for practice on day one of residency. Activities will include simulations and other interactive learning modalities to address the core entrustable professional activities for entering residency. Possible topics will include:
- Assessment of moderate to high complexity patients
- Order writing and prescription writing
- Giving and receiving patient handovers
- Recognizing a patient requiring urgent or emergent care and initiating management
- Interprofessional collaboration on a team
Integrated Curricular Elements Program
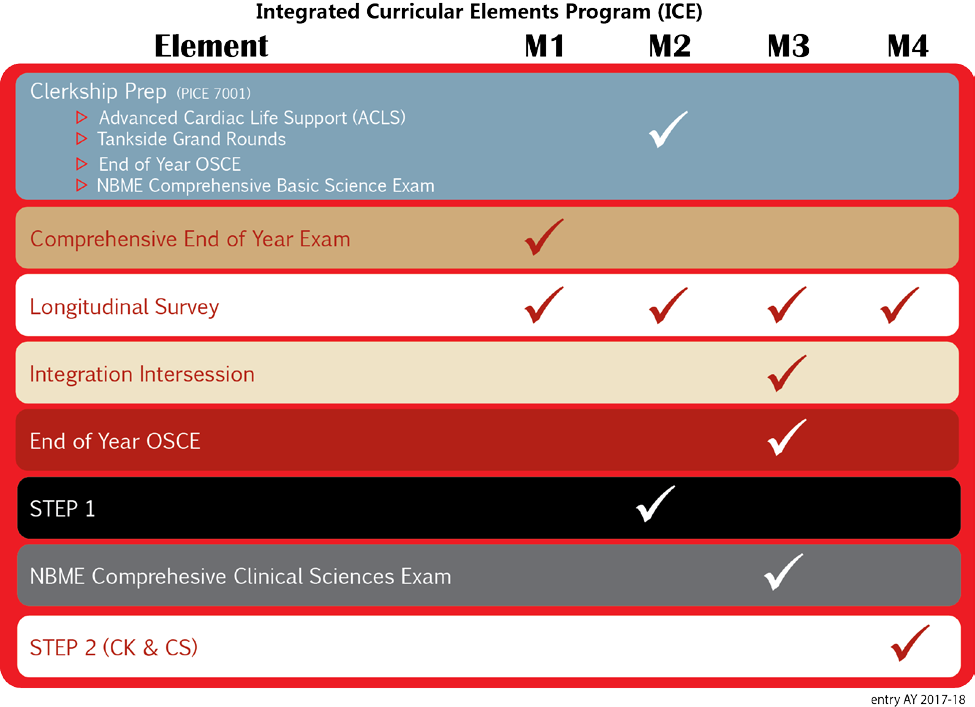
The Integrated Curricular Elements (ICE) Program contains curricular requirements that intentionally span the pre-clerkship and clerkship phases. ICE requirements occur in each year. There are credit and non-credit components of the ICE program.
The Clerkship Prep Course (PICE 7001) is an eight-week credit-based course occurring at the end of the MS2 year, which ensures students possess the essential knowledge and skills required for entry into the clerkship phase of their medical training. The major elements of this course include Advanced Cardiovascular Life Support (ACLS) training, Tankside Grand Rounds (TSGR), an Objective Structured Clinical Examination (OSCE), a self-directed learning phase, and the National Board of Medical Examiners’ Comprehensive Basic Science Exam (NBME CBSE).
The integrated curricular elements are graduation requirements and students are expected to complete them as scheduled within the years as indicated and in the framework as described. As with all of the courses and requirements, please consult the relevant syllabi and descriptions in the curriculum management system for additional information.
The Clerkship Prep Course and other ICE Program elements are outlined in the table below:
In addition, non-curricular elements (like holidays) may be placed on the ICE calendars so that you can plan for them.
Year 3 Intersessions:
Two one-week intersessions in the third year are scheduled following Block 2 and following Block 3. The entire class will participate in the activities. Content will integrate the experiences in the clinical rotations during Year 3 with concepts from the Year 1 &2 coursework.
Topics may include:
- Ethics and professionalism
- Personal reflection
- Biostatistics and Epidemiology
- Cultural competency
- Basic science material
- Integrated case presentations
- Medical skills
Content in the intercessions is designed to allow for flexibility in order to adapt to the needs of the class, prepare the students for 4th year, as well as national examinations, such as the USMLE Step 2 CK and CS.
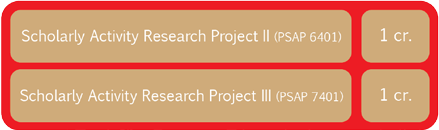
Scholarly Activity and Research Program
The Scholarly Activity and Research Program (SARP) (PSAP 5401, 6401, 7401) provides medical students with an opportunity to design and execute an independent scholarly project or research project under the guidance of a faculty mentor. A wide variety of topics and research areas are available in three broad categories, allowing for a project to be tailored to a student’s background and interests: 1) basic, clinical and translational research; 2) epidemiology, community-based, behavior, public and environmental health; and 3) medical humanities, qualitative research and medical education research. This is a three credit (pass/fail) mandatory curriculum requirement, with one credit awarded for selection of a mentor and preparation of a project plan, one credit for execution and final report of the project itself, and a final credit awarded for a poster summarizing the project presented at an annual student symposium held in the fall semester.
Students can choose between one of three tracks for completing their SARP requirement. Track 1 concentrates execution of the project into the summer between the first and second year with a final report and poster presented in the fall of the second year; whereas Track 2 provides the student more flexibility in the execution of their project with completion and final report and poster presentation in the fall of the third year. Track 3 is dedicated to completion of the SARP requirement by the spring of year four. Students on Track 2 or Track 3 are required to submit annual progress reports until their SARP requirement is completed.
For all tracks, selection of a mentor and preparation of a project plan is due at the end of the first year. This introduction to the methodology and analytic thinking involved with scholarly activity and research is designed to enhance the medical training experience and provide an appreciation for the tight integration between scholarship, research and clinical practice. Students who excel in scholarly activities and research, based on the judgment of a faculty panel, are eligible for special recognition at graduation with the notation of graduating with Distinction in Research and Scholarship on their diploma.
The M.D. degree will be awarded to students who satisfactorily complete the following:
- all required courses and clerkships
- all graduation requirements
- passing the United States Medical Licensing Examination (USMLE) Steps 1 and 2 (Clinical Knowledge & Clinical Skills components) exams
Interprofessional Education First year medical students are required to complete the TTUHSC online course for preparation for interprofessional education. This requirement is coordinated through the Society, Community and Individual Couse (PSCI 5211) during immersion.
United States Medical Licensing Examination (USMLE) In order to become fully licensed to practice medicine in the United States, individuals must pass all four USMLE Step exams – Step 1, Step 2 Clinical Knowledge, Step 2 Clinical Skills, and Step 3. Each state’s medical licensing board determines the number of attempts individuals may make at each Step in order to remain eligible for licensure. In Texas, individuals are limited to three attempts on each Step. To learn more about USMLE policies view the PLFSOM Student Handbook (Step I Exam, Step II Exam) published annually by the Office of Student Affairs.
